Testicular Cancer
About Testicular Cancer
Key Points
- Testicular cancer is a disease in which malignant (cancer) cells form in the tissues of one or both testicles.
- Health history can affect the risk of testicular cancer.
- Signs and symptoms of testicular cancer include swelling or discomfort in the scrotum.
- Tests that examine the testicles and blood are used to detect (find) and diagnose testicular cancer.
- Certain factors affect prognosis (chance of recovery) and treatment options.
- Treatment for testicular cancer can cause infertility.
Testicular cancer is a disease in which malignant (cancer) cells form in the tissues of one or both testicles.
The testicles are 2 egg-shaped glands located inside the scrotum (a sac of loose skin that lies directly below the penis). The testicles are held within the scrotum by the spermatic cord, which also contains the vas deferens and vessels and nerves of the testicles.
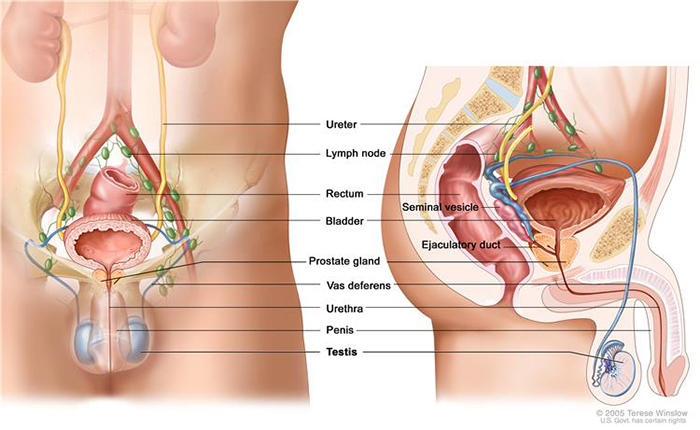
Anatomy of the male reproductive and urinary systems, showing the testicles, prostate, bladder, and other organs.
The testicles are the male sex glands and produce testosterone and sperm. Germ cells within the testicles produce immature sperm that travel through a network of tubules (tiny tubes) and larger tubes into the epididymis (a long coiled tube next to the testicles) where the sperm mature and are stored.
Almost all testicular cancers start in the germ cells. The two main types of testicular germ cell tumours are seminomas and non-seminomas. These 2 types grow and spread differently and are treated differently. Non-seminomas tend to grow and spread more quickly than seminomas. Seminomas are more sensitive to radiation. A testicular tumour that contains both seminoma and non-seminoma cells is treated as a non-seminoma.
Testicular cancer is the most common cancer in men 20 to 35 years old.
Signs and symptoms of testicular cancer include swelling or discomfort in the scrotum.
These and other signs and symptoms may be caused by testicular cancer or by other conditions. Check with your doctor if you have any of the following:
- A painless lump or swelling in either testicle.
- A change in how the testicle feels.
- A dull ache in the lower abdomen or the groin.
- A sudden build-up of fluid in the scrotum.
- Pain or discomfort in a testicle or in the scrotum.
Certain factors affect prognosis (chance of recovery) and treatment options.
The prognosis (chance of recovery) and treatment options depend on the following:
- Stage of the cancer (whether it is in or near the testicle or has spread to other places in the body, and blood levels of AFP, β-hCG, and LDH).
- Type of cancer.
- Size of the tumour.
- Number and size of retroperitoneal lymph nodes.
Testicular cancer can usually be cured in patients who receive adjuvant chemotherapy or radiation therapy after their primary treatment.
Treatment for testicular cancer can cause infertility.
Certain treatments for testicular cancer can cause infertility that may be permanent. Patients who may wish to have children should consider sperm banking before having treatment. Sperm banking is the process of freezing sperm and storing it for later use.
See the PDQ summary on Sexuality and Reproductive Issues for more information.
Health history can affect the risk of testicular cancer.
Anything that increases the chance of getting a disease is called a risk factor. Having a risk factor does not mean that you will get cancer; not having risk factors doesn’t mean that you will not get cancer. Talk with your doctor if you think you may be at risk. Risk factors for testicular cancer include:
- Having had an undescended testicle.
- Having had abnormal development of the testicles.
- Having a personal history of testicular cancer.
- Having a family history of testicular cancer (especially in a father or brother).
- Being white.
Stages of Testicular Cancer
Key Points
- After testicular cancer has been diagnosed, tests are done to find out if cancer cells have spread within the testicles or to other parts of the body.
- There are three ways that cancer spreads in the body.
- Cancer may spread from where it began to other parts of the body.
- The following stages are used for testicular cancer:
- Stage 0 (Testicular Intraepithelial Neoplasia)
- Stage I
- Stage II
- Stage III
There are three ways that cancer spreads in the body.
Cancer can spread through tissue, the lymph system, and the blood:
- Tissue. The cancer spreads from where it began by growing into nearby areas.
- Lymph system. The cancer spreads from where it began by getting into the lymph system. The cancer travels through the lymph vessels to other parts of the body.
- Blood. The cancer spreads from where it began by getting into the blood. The cancer travels through the blood vessels to other parts of the body.
Cancer may spread from where it began to other parts of the body.
When cancer spreads to another part of the body, it is called metastasis. Cancer cells break away from where they began (the primary tumour) and travel through the lymph system or blood.
- Lymph system. The cancer gets into the lymph system, travels through the lymph vessels, and forms a tumour (metastatic tumour) in another part of the body.
- Blood. The cancer gets into the blood, travels through the blood vessels, and forms a tumour (metastatic tumour) in another part of the body.
The following stages are used for testicular cancer:
Stage 0 (Testicular Intraepithelial Neoplasia)
In stage 0, abnormal cells are found in the tiny tubules where the sperm cells begin to develop. These abnormal cells may become cancer and spread into nearby normal tissue. All tumour marker levels are normal. Stage 0 is also called testicular intraepithelial neoplasia and testicular intratubular germ cell neoplasia.
Stage I
In stage I, cancer has formed. Stage I is divided into stage IA, stage IB, and stage IS and is determined after an inguinal orchiectomy is done.
- In stage IA, cancer is in the testicle and epididymis and may have spread to the inner layer of the membrane surrounding the testicle. All tumour marker levels are normal.
- In stage IB, cancer:
- is in the testicle and the epididymis and has spread to the blood vessels or lymph vessels in the testicle; or
- has spread to the outer layer of the membrane surrounding the testicle; or
- is in the spermatic cord or the scrotum and may be in the blood vessels or lymph vessels of the testicle.
All tumour marker levels are normal.
- In stage IS, cancer is found anywhere within the testicle, spermatic cord, or the scrotum and either:
- all tumour marker levels are slightly above normal; or
- one or more tumour marker levels are moderately above normal or high.

Pea, peanut, walnut, and lime show tumour sizes.
Stage II
Stage II is divided into stage IIA, stage IIB, and stage IIC and is determined after an inguinal orchiectomy is done.
- In stage IIA, cancer:
- is anywhere within the testicle, spermatic cord, or scrotum; and
- has spread to up to 5 lymph nodes in the abdomen, none larger than 2 centimetres.
All tumour marker levels are normal or slightly above normal.
- In stage IIB, cancer is anywhere within the testicle, spermatic cord, or scrotum; and either:
- has spread to up to 5 lymph nodes in the abdomen; at least one of the lymph nodes is larger than 2 centimetres, but none are larger than 5 centimetres; or
- has spread to more than 5 lymph nodes; the lymph nodes are not larger than 5 centimetres.
All tumour marker levels are normal or slightly above normal.
- In stage IIC, cancer:
- is anywhere within the testicle, spermatic cord, or scrotum; and
- has spread to a lymph node in the abdomen that is larger than 5 centimetres.
All tumour marker levels are normal or slightly above normal.
Stage III
Stage III is divided into stage IIIA, stage IIIB, and stage IIIC and is determined after an inguinal orchiectomy is done.
- In stage IIIA, cancer:
- is anywhere within the testicle, spermatic cord, or scrotum; and
- may have spread to one or more lymph nodes in the abdomen; and
- has spread to distant lymph nodes or to the lungs.
Tumour marker levels may range from normal to slightly above normal.
- In stage IIIB, cancer:
- is anywhere within the testicle, spermatic cord, or scrotum; and
- may have spread to one or more lymph nodes in the abdomen, to distant lymph nodes, or to the lungs.
The level of one or more tumour markers is moderately above normal.
- In stage IIIC, cancer:
- is anywhere within the testicle, spermatic cord, or scrotum; and
- may have spread to one or more lymph nodes in the abdomen, to distant lymph nodes, or to the lungs.
The level of one or more tumour markers is high or cancer:
- is anywhere within the testicle, spermatic cord, or scrotum; and
- may have spread to one or more lymph nodes in the abdomen; and
- has not spread to distant lymph nodes or the lung but has spread to other parts of the body.
Tumour marker levels may range from normal to high.
Recurrent Testicular Cancer
Recurrent testicular cancer is cancer that has recurred (come back) after it has been treated. The cancer may come back many years after the initial cancer, in the other testicle or in other parts of the body.
Testicular Cancer Diagnosis and Screening
Ultrasound
Ultrasound is a procedure in which high-energy sound waves (ultrasound) are bounced off internal tissues or organs and make echoes. The echoes form a picture of the body tissues called a sonogram.
CT Scan (chest/abdomen)
CT scan is basically an x-ray tube that rotates in a circle around the patient and takes a series of pictures as it rotates. The multiple x-ray pictures are reconstructed by a computer in axial slice images at different levels. Each level can be examined separately.
A CT scan may show if the cancer has spread to other parts of the body such as the lymph nodes.
The scan takes from 10-30 minutes. You may be given a drink or injection of a dye, which allows particular areas to be seen more clearly. For a few minutes, this may make you feel hot all over. If you are allergic to iodine or have asthma you could have a more serious reaction to the injection, so it is important to let your doctor know beforehand. You will probably be able to go home as soon as the scan is over.
Pathology
There are several tumour markers that may be associated with testicular cancer (αFP, βHCG, LDH). These may be measured in the blood and Prof Patel will discuss with you whether these tests are required.
Testicular Cancer Treatments
Surgery
A biopsy of the suspect tissue can provide an absolute diagnosis of testicular cancer. If a suspicious mass is found and other conditions are ruled out surgery is the most common form of treatment for most testicular cancers. There are two main types of surgery depending on the type of cancer that is found.
Orchidectomy
Orchidectomy involves the surgical removal of the testicle. This procedure is performed in hospital under general anaesthetic. An incision is made into the groin, where the blood vessel leading to the testicle is first cut off in a bid to prevent cancer cells ‘spilling’ into the rest of the body.The procedure takes approximately an hour to perform and requires a short stay at the hospital. Most patients have a full recovery in 2 to 4 weeks.
Side effects
Most side effects from this surgery tend to be temporary. Typically pain and discomfort around the operation site are the most common side effects, but this pain can be managed with painkillers, and should subside over time.
If you have had one testicle removed a prosthetic testicle can be made and inserted into the scrotum at a later date; sexuality and fertility should not be affected.
Removing both testicles leads to infertility. Hormone therapy may be needed to replace the lack of testosterone production; taking hormones will mean that sexual activity can continue and that erections and ejaculation will still be possible – although no sperm will be produced.
Talk to Prof Patel about possible side effects and the methods available to alleviate them.
Retroperitoneal Lymph Node Dissection (RPLND)
Depending on the type and stage of the cancer, some lymph nodes at the back of the abdomen (around the large blood vessels known as the aorta and inferior vena cava) may also be removed at the same time as the orchidectomy or during a second operation. Not all patients with testicular cancer need to have lymph nodes removed, so it’s important to discuss this (and the possible alternatives) with Prof Patel.
RPLND is a complex and long operation. A large incision is typically made down the middle of the abdomen to remove the lymph nodes. It should be performed by a surgeon who has significant experience in the procedure as it is very complex.
Side effects
Most side effects from this surgery tend to be temporary. Typically pain and discomfort around the operation site are the most common side effects, but this pain can be managed with painkillers, and should subside over time.
Surgery to remove retroperitoneal lymph nodes is a major operation. Serious complications are not common, but they can happen. About 5% to 10% of patients have temporary complications after surgery, such as bowel obstruction or wound infections. The standard approach for an RPLND requires a large incision in the abdomen, which will leave a scar and can take some time to heal. Mobility will be limited for some time after the operation. This is less likely with laparoscopic surgery, which uses smaller incisions.
This type of surgery does not cause impotence – a man can still have erections and sexual intercourse. But it might damage some of the nerves that control ejaculation. If these nerves are damaged, when a man ejaculates, the semen is not propelled forward through the urethra to exit the body but rather goes backwards into the bladder. This is known as retrograde ejaculation, and it can make it hard to father children.
To save the normal ejaculation function, surgeons have developed a type of retroperitoneal lymph node surgery called nerve-sparing surgery that is very successful when done by experienced doctors. Testicular cancer often affects men at an age when they may be trying to have children. These men may wish to discuss nerve-sparing surgery with their doctors, as well as sperm banking (freezing and storing sperm cells obtained before treatment).
Chemotherapy
This is commonly used in the treatment of testicular cancer that has spread beyond the testicle. In some cases it is used when the cancer appears to be still confined to the testicle.
If chemotherapy is necessary, Prof Patel will refer you to a medical oncologist working as part of his team, who specialises in the management of testicular cancer.
Testicular cancer is usually very responsive to chemotherapy, resulting in very high cure rates.
What is chemotherapy?
Chemotherapy concerns the use of special cytotoxic drugs to treat cancers by either killing the cancer cells or slowing their growth. Chemotherapy drugs travel round the body and attack rapidly growing cells, which may also include healthy cells in the body as well as cancer cells. However the breaks between bouts of chemo allow the bodies normal cells to recover before the next course of chemo.
To travel the body, chemotherapy needs to enter the bloodstream and the quickest way to do this is intravenously – through a vein or artery. Other methods of administering chemotherapy may also take the form of intra-muscular injections, tablets or creams. The way you have chemotherapy depends on a number of factors including the type of cancer you have and the drugs that you are taking. Talk with your doctor if you have any questions about your treatment regime.
Some cancers can be treated or cured by chemotherapy alone, while some treatments may combine chemotherapy with other procedures such as surgery or radiotherapy – this is known as adjuvant therapy. Adjuvant chemotherapy can be used before the main treatment to help make the tumour smaller, or after treatment to kill residual cancer cells that may cause problems later in treatment.
In some instances chemotherapy may not be able to control the cancer but may be used to relieve symptoms such as pain and help you lead as normal a life as is possible.
There are many different combinations of chemotherapy used to treat various cancers, and these may have different effects on different people.
Side effects of chemotherapy
While chemotherapy is useful for the killing of cancer cells in the body, as with most other treatments patients may experience side effects from the chemotherapy. These side effects vary from treatment to treatment and from person to person but fortunately these problems may disappear with time or be managed to reduce the impact that they may cause.
The most common side effects are nausea and vomiting, fatigue (tiredness), alopecia (hair loss), muscular, nerve and blood effects as well as bowel (constipation or diarrhoea) and oral problems.
It is important that you tell the doctors and nurses if you are experiencing any side effects from your treatment so that they can discuss an appropriate course of action with you.
Treatment Options by Stage
Stage 0 (Testicular Intraepithelial Neoplasia)
Treatment of stage 0 may include the following:
- Radiation therapy.
- Surveillance.
- Surgery to remove the testicle.
Stage I Testicular Cancer
Treatment of stage I testicular cancer depends on whether the cancer is a seminoma or a non-seminoma.
Treatment of seminoma may include the following:
- Surgery to remove the testicle, followed by surveillance.
- For patients who want active treatment rather than surveillance, treatment may include:
- Surgery to remove the testicle, followed by chemotherapy.
Treatment of non-seminoma may include the following:
- Surgery to remove the testicle, with long-term follow-up.
- Surgery to remove the testicle and lymph nodes in the abdomen, with long-term follow-up.
- Surgery followed by chemotherapy for patients at high risk of recurrence, with long-term follow-up.
Stage II Testicular Cancer
Treatment of stage II testicular cancer depends on whether the cancer is a seminoma or a non-seminoma.
Treatment of seminoma may include the following:
- When the tumour is 5 centimetres or smaller:
- Surgery to remove the testicle, followed by radiation therapy to lymph nodes in the abdomen and pelvis.
- Combination chemotherapy.
- Surgery to remove the testicle and lymph nodes in the abdomen.
- When the tumour is larger than 5 centimetres:
- Surgery to remove the testicle, followed by combination chemotherapy or radiation therapy to lymph nodes in the abdomen and pelvis, with long-term follow-up.
Treatment of non-seminoma may include the following:
- Surgery to remove the testicle and lymph nodes, with long-term follow-up.
- Surgery to remove the testicle and lymph nodes, followed by combination chemotherapy and long-term follow-up.
- Surgery to remove the testicle, followed by combination chemotherapy and a second surgery if cancer remains, with long-term follow-up.
- Combination chemotherapy before surgery to remove the testicle, for cancer that has spread and is thought to be life-threatening.
Stage III Testicular Cancer
Treatment of stage III testicular cancer depends on whether the cancer is a seminoma or a non-seminoma.
Treatment of seminoma may include the following:
- Surgery to remove the testicle, followed by combination chemotherapy. If there are tumours remaining after chemotherapy, treatment may be one of the following:
- Surveillance with no treatment unless tumours grow.
- Surveillance for tumours smaller than 3 centimetres and surgery to remove tumours larger than 3 centimetres.
- A PET scan two months after chemotherapy and surgery to remove tumours that show up with cancer on the scan.
- A clinical trial of chemotherapy.
Treatment of non-seminoma may include the following:
- Surgery to remove the testicle, followed by combination chemotherapy.
- Combination chemotherapy followed by surgery to remove the testicle and all remaining tumours. Additional chemotherapy may be given if the tumour tissue removed contains cancer cells that are growing or if follow-up tests show that cancer is progressing.
- Combination chemotherapy before surgery to remove the testicle, for cancer that has spread and is thought to be life-threatening.
- A clinical trial of chemotherapy.
Treatment Options for Recurrent Testicular Cancer
Treatment of recurrent testicular cancer may include the following:
- Combination chemotherapy.
- High-dose chemotherapy and stem cell transplant.
- Surgery to remove cancer that has either:
- come back more than 2 years after complete remission; or
- come back in only one place and does not respond to chemotherapy.
- A clinical trial of a new therapy.